The Arthritis Newsletter
Winter 2015Motherhood and Thrombophlebitis
By Marilyn Mulldoon
I entered the realm of motherhood rather late. Like many other creatures, I guess I just didn’t breed well in
captivity. Joking aside, I did not get around to reproducing until my 37th year when my Sjögren’s syndrome
was already present but not yet diagnosed. And in spite of my age, I experienced a normal pregnancy
except for a little elevated blood pressure.
The lineage of women with varicose veins in my family is legendary. I have had varicosity issues since my
late teens, and I really didn’t think my legs looked any worse during my pregnancy – well not until I went
into labour. I awoke at 2:00 a.m. and quickly realized that the “big show” had started. With only two hours of
sleep, I was not prepared for the next 18 sleepless hours of labour. I had done the prenatal classes and
knew how to breathe, but push? Nothing prepares you for the amount of exertion required to “move things
along”. After 45 minutes in the delivery suite, we were done.
Following the birth, and in spite of complete physical exhaustion, I could not sleep. I worried about how to
look after this new person who had the gall to arrive without any sort of owner’s manual or instruction kit.
Eventually, after only a short rest, I turned on the lights to check why my legs, my left leg in particular, were
becoming so painful and tender. I was shocked to see the state of my veins – they were turning black!
I buzzed for the nurse, who sent for the doctor, who quickly sent for anti-embolism stockings. Every so
often a nurse would ask me to pump my ankles up and down. They were concerned about deep vein
thrombosis. Satisfied that I had upper superficial thrombophlebitis, they measured my legs, and I sat in bed
dressed in uncomfortable stockings, with aching legs and a hungry newborn all the while wondering if I
would die from a blood clot. Aspirin, at the time, was the first line of treatment for thrombosis, but nursing
mothers cannot take Aspirin because of the possible development of Reye’s syndrome in their babies. At
this point, I would have done anything for a decent sleep, a nanny and new legs.
By morning, my left leg no longer felt like it was part of my body. It was a dead weight, and I had to drag it
around for the next two weeks until the feeling slowly returned. I am thankful that the antinuclear
antibodies (ANA) from my Sjögren’s syndrome did not pass the placenta. The presence of ANA in the fetal
circulation may lead to congenital heart block requiring a pacemaker immediately following birth. The fear
of thrombosis was enough postnatal drama!
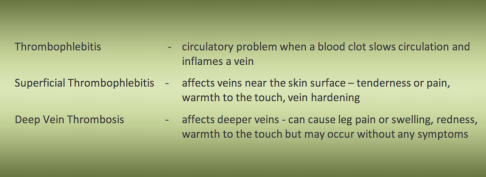
Why did I get thrombophlebitis? Certain risk factors appear to increase the risk: trauma, childbirth, and
varicose veins. Pregnancy and/or postpartum vein inflammation are not uncommon. Unlike when I had my
baby, today we have more awareness, vascular specialists to work with the general practitioner or OB/GYN
(physician specializing in obstetrics and gynecology), and improved antiembolism stockings to help with
swelling and inflammation. Perhaps my undiagnosed inflammatory arthritis also contributed to my problem.
Other possible causes of thrombophlebitis are: blood stasis, blood vein injury, increased blood clotting,
indwelling catheters, and infection.
Needless to say, I learned it is important to keep an eye on vein activity. Spider veins are rarely a serious
health problem; however, varicose veins sometimes lead to more serious health problems. Varicose veins
can be properly monitored by any of these specialists:
- A vascular medicine doctor
- A vascular surgeon
- A dermatologist
- A phlebologist (vein specialist)
And don’t forget, whether we’re being treated for veins or arthritis, let’s keep on moving!